Over the past year, Doctors Without Borders/Médecins Sans Frontières (MSF) has responded to the unprecedented threats posed by COVID-19 across all our projects. We also see how the pandemic can compound existing problems, trigger new crises, and overshadow other humanitarian needs.
For this special edition of Alert, we highlight some of the world's forgotten emergencies—forgotten by many in the international community but certainly not by our teams on the ground. In this photo essay, we bear witness to suffering, survival, and extraordinary strength during a tumultuous year.
Just days after the first COVID-19 cases were reported in Puerto Rico in mid-March, the governor imposed a lockdown—among the strictest measures anywhere in the United States. So when Doctors Without Borders/Médecins Sans Frontières (MSF) began exploring the need for an emergency response on the island, we relied heavily on local networks for advice.
For MSF, the first step before responding to any crisis is to evaluate the needs. This exploratory mission—or explo, for short—is typically carried out by staff already working in the area or specialists sent from headquarters.
This time we reached out to Sophie Delaunay, a former executive director of MSF-USA with more than 20 years of experience with the organization, and who now lives in San Juan. “So, it’s very difficult to move around,” she said, recalling conditions at the beginning of the lockdown. “I’m reaching out to organizations that are already on the ground. Because that was the best way for us to do an assessment—to figure out who was doing what, where the needs and the gaps were.” Delaunay eventually formed a nine-member team to help with the emergency response— all recruited from Puerto Rico.
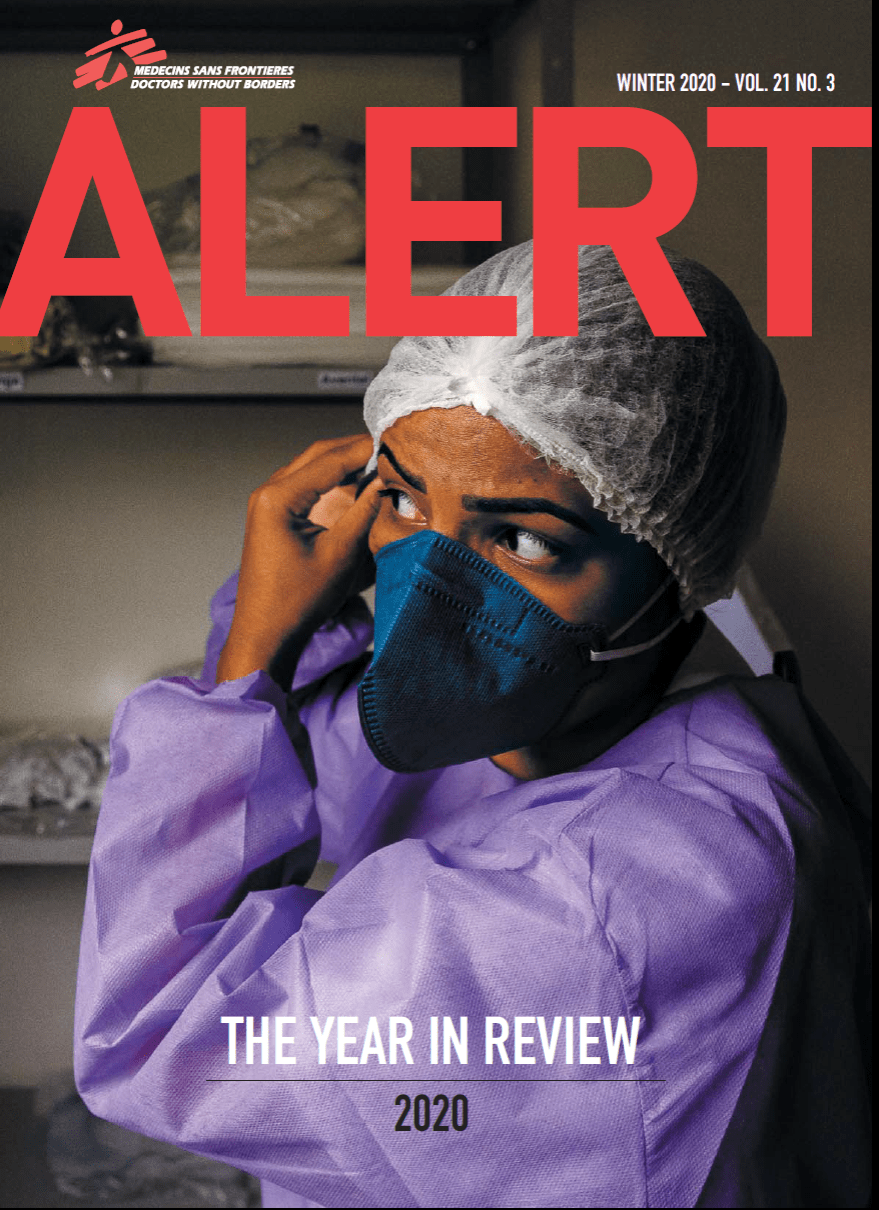
The most immediate need, as in most places around the world, was for personal protective equipment (PPE) for frontline health workers. So we started with the distribution of N95 masks, donated by San Francisco-based nonprofit organization HumankindNOW. The team eventually delivered over 30,000 PPE items to health care facilities— including hospitals, medical universities, emergency rooms, and blood banks.

We also identified deeper needs among neglected and marginalized communities, for whom COVID-19 has only aggravated the risks. “Prior to the pandemic, the health care system had many problems,” said Dr. Jonathan Caldera, who was hired as the MSF physician. “Those who were already in need in our community, when the pandemic came, it became much more difficult for them.”
MSF worked closely with community leaders from across the island to reach people who were cut off from essential health care services. We partnered with several local organizations—including Taller Salud, a group focused on improving women’s access to health care; Coalicion de Coaliciones, which provides services to homeless people; and Intercambios, which runs needle-exchange and harm reduction programs for people who use drugs.

The MSF team began offering home-based primary care services as well as monitoring for COVID-positive patients. Over three-and-a-half months we provided medical consultations to more than 1,200 patients, mostly older adults suffering from chronic conditions like diabetes and hypertension, which can make them even more vulnerable to the disease. In addition we supported 80 patients through our COVID monitoring program, which consisted of a 14-day check-in system for individuals who tested positive but had mild, moderate, or no symptoms. An MSF nurse checked in daily with each patient via text message, offering medical advice as well as psychosocial support. If a patient’s symptoms worsened, they were referred to a hospital or a primary care doctor.
MSF mobile medical teams traveled to isolated communities such as Buen Consejo in Rio Piedras, Puerto Rico. “There is a large aging population who are practically alone,” said Rolando Betancourt, a nurse on the MSF team. “Many houses do not have potable water, nor do they have basic sanitation services.”

With an ongoing crisis like the COVID-19 pandemic, it can be especially difficult to know when it’s time to close a project. By late September, it seemed as if the acute phase of the emergency in Puerto Rico had passed. Yet the crisis had exposed some of the chronic needs and systemic failures that demand sustained attention.
Betancourt and two other members of the original MSF team decided to form a new organization to continue to provide essential medical services: Puerto Rico Salud.
“We know that the crisis is not over, and that many people in Puerto Rico do not have adequate access to health care,” said Delaunay. “But we close our program with a sense of reassurance that the very next day after MSF leaves, Puerto Rico Salud will continue this lifesaving work.”
When MSF closes a project, we generally seek a local partner or government agency able to carry on the activities in order to execute a successful “handover”. The ideal scenario is that when our immediate medical objectives have been reached, medical activities can continue even without MSF’s direct intervention and resources. Puerto Rico Salud stepped in at a critical moment to make this a smooth transition.
Betancourt said he was personally moved to see how many people on the island were struggling to survive without access to basic health services. “We set out to find a way to be able to continue the same work, with the same quality standards,” he said, “to reach the people who need it for a long time to come.”