Viral load testing shows the amount of HIV in the blood of a person living with the virus. Antiretroviral drugs suppress HIV replication. If a person on ARV treatment has a viral load above a certain point, it indicates that the treatment isn’t working, either because the medicines aren’t being taken correctly, or because HIV has become resistant to the antiretroviral medicines.
In either case, health workers can respond quickly, working with people on treatment to improve adherence to a drug regimen or prescribing advanced "second-line" drugs. These steps can bring viral load down to virtually "undetectable" levels, helping those on treatment stay healthy and benefiting the community by reducing the risk of transmission. Sexual transmission of HIV is 96 percent less likely when viral load is undetectable.
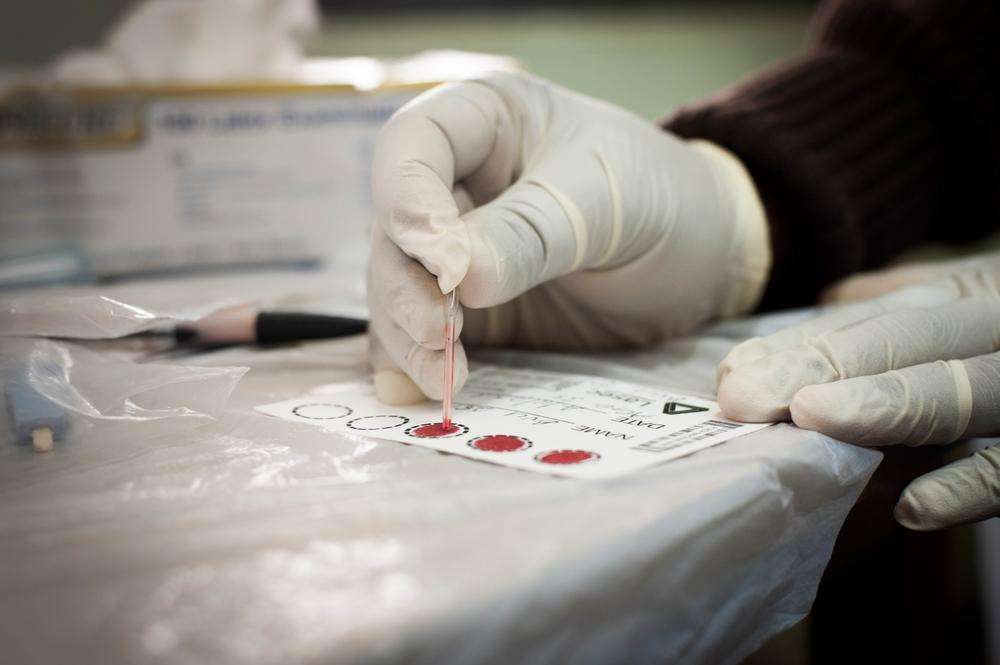
Viral load testing is the gold standard for monitoring the health of people on HIV treatment. But because the equipment can be expensive and requires skilled staff, the test is not widely available in poor countries with limited resources.
Doctors Without Borders/Médecins Sans Frontières (MSF)—thanks to co-funding from UNITAID—is working to develop ways to expand viral load testing in eight countries in sub-Saharan Africa, including MSF sites in the Democratic Republic of Congo, Lesotho, Malawi, Mozambique, South Africa, Swaziland, Uganda, and Zimbabwe. These photographs offer a glimpse of MSF viral load and HIV treatment projects in Malawi, where the HIV adult prevalence is high at about 14–16 percent.