Workey Mekonen was sleeping on the ground in a farm shed in northern Ethiopia’s Amhara region when she woke up to a sudden piercing pain in her forehead. She caught sight of a snake slithering away. Relieved at first that it was only a small snake, the pain and swelling soon made her fear for her life.
Workey, age 24, earns a meager living for herself and her four children by cooking for farm workers in the fields. Fellow laborers took Workey to her uncle, who took her to a clinic run by Doctors Without Borders/Médecins Sans Frontières (MSF) in nearby Abdurafi town. By that time, Workey’s face was so swollen that she could not see.
Workey’s test result showed no blood clotting, a clear indicator that the snake had injected its venom, and that this young woman needed urgent treatment. “The first ten minutes are critical and need close monitoring to ensure that she has no harmful reactions to the antivenom,” said MSF clinical officer Degifew Dires. “Over the coming hours, we will regularly check her physical condition and vital signs.”
Fortunately, she made a full recovery and was discharged from the clinic after five days. MSF doctor Ernest Nshimiyimana said Workey is one of the lucky ones. “Effective antivenom is either unavailable or is too expensive for the communities most affected by snakebite,” he said.
Every year, an estimated 2.7 million people are bitten by venomous snakes, resulting in death for more than 100,000 people and life-long disfigurement and disability for 400,000 more. MSF teams witness the devastating impact of snakebites on victims, their families, and communities. Victims can suffer a variety of immediate physical effects, including suffocation, bleeding disorders, kidney failure, and severe tissue damage that can require amputation. In 2017, more than 3,000 patients were admitted to MSF-supported hospitals for snakebite treatment, mainly in sub-Saharan Africa and in the Middle East.
And this may only be a fraction of the cases worldwide. Hospital records are an unreliable guide because many people bitten by snakes never make it to the hospital for treatment. Snakebite hits the poorest of the poor: farmers who work barefoot in the fields and people living in remote rural areas with limited access to health education and medical care. Displaced people fleeing conflict or violence who may hide out in snake habitats are also at risk. Children, due to their smaller body mass, are particularly vulnerable to death and disability from snakebite poisoning.
The vast majority of snakebite victims are unable to access affordable and effective treatment for a variety of reasons, including high prices for antivenoms, unavailability of effective antivenom in remote places when urgently needed, and lack of skilled health care workers. Many families are driven into debt and destitution in their attempts to get treatment. Death and disability can also spell financial ruin. Stigma and discrimination against disabled snakebite survivors are commonplace.
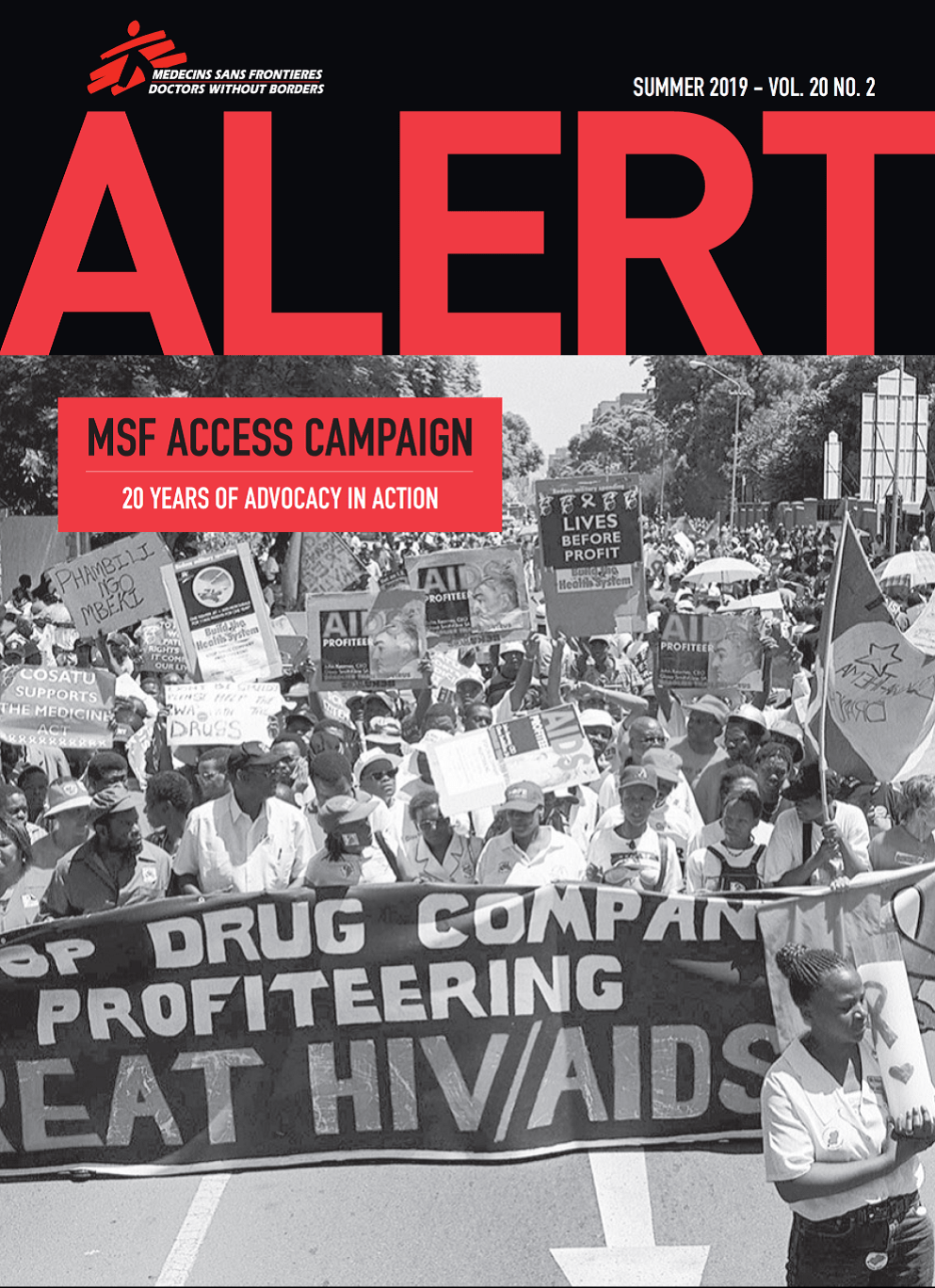
For years MSF’s Access Campaign has been calling for greater efforts to prevent and control snakebite envenoming. In 2017, the World Health Organization (WHO) recognized snakebite envenoming on its list of Neglected Tropical Diseases, and this May released its roadmap to address this major public health crisis. MSF is pushing for more attention to snakebite in fragile states and conflict zones, and for an adequate stockpile of quality-assured antivenoms.
MSF is cautiously optimistic that the WHO roadmap could be a turning point in tackling snakebite. The roadmap includes ambitious targets for reducing death and disability from snakebite, as well as outlining the funding needed to deliver on these plans. It finally provides a framework for MSF and other actors to mobilize governments and donors to respond to snakebite with the urgency and attention that this neglected public health crisis demands.
Now governments and donors need to pledge enough funds to scale up effective interventions, in particular technical assistance for countries to roll out the roadmap; procurement and supply of affordable, quality assured antivenom products; and a dramatic reduction of out-of-pocket costs for snakebite victims, for whom access is a matter of life or death.
“Imagine how frightening it must be to be bitten by a snake,” said Dr. Gabriel Alcoba, MSF medical advisor on snakebite, “to feel the pain and venom spread through your body—knowing it may kill you and there is no treatment available, or that you can’t afford to pay for it.”
We can imagine a better future for snakebite victims, and working together we can ensure that they get the care and treatment they deserve.