Doctors Without Borders/Médecins Sans Frontières (MSF) relies on the dedicated efforts of over 10,000 nurses worldwide—the largest professional group within our operations—to provide critical health care services. In recognition of International Nurses Day, MSF is drawing attention to the vital role nurses play in our intensive care units (ICUs). These nurses offer essential care to seriously ill patients who might otherwise have no access to lifesaving treatment.
In emergency situations like the COVID-19 pandemic and Ebola outbreaks, MSF’s ICUs are set up to provide immediate critical care. In longer-term projects, MSF’s ICU teams treat surgical patients with burns or conflict-related injuries, women experiencing complications of pregnancy or childbirth, and severely sick children, particularly those under five years old, who make up the majority of our patients. We also provide specialized care for severely sick newborns.
In many countries, training standards for health care professionals can vary widely, and nurses often acquire new skills on the job. In some regions, there may be no referral options available for higher levels of care. In other areas, MSF may introduce materials and equipment that local health care providers have not used before. While each context we work in presents unique challenges, one common theme is that patients’ needs are often greater than the resources available.
Despite these challenges, we’re always working to meet the complex needs of our patients. MSF nurses strive to provide the best possible person- and community-centered nursing care, even in the most difficult circumstances. Here, MSF nurses from Bangladesh, Haiti, Nigeria, and Yemen describe the challenges they have faced and the achievements they have made in caring for their patients, as well as their vision for the future.
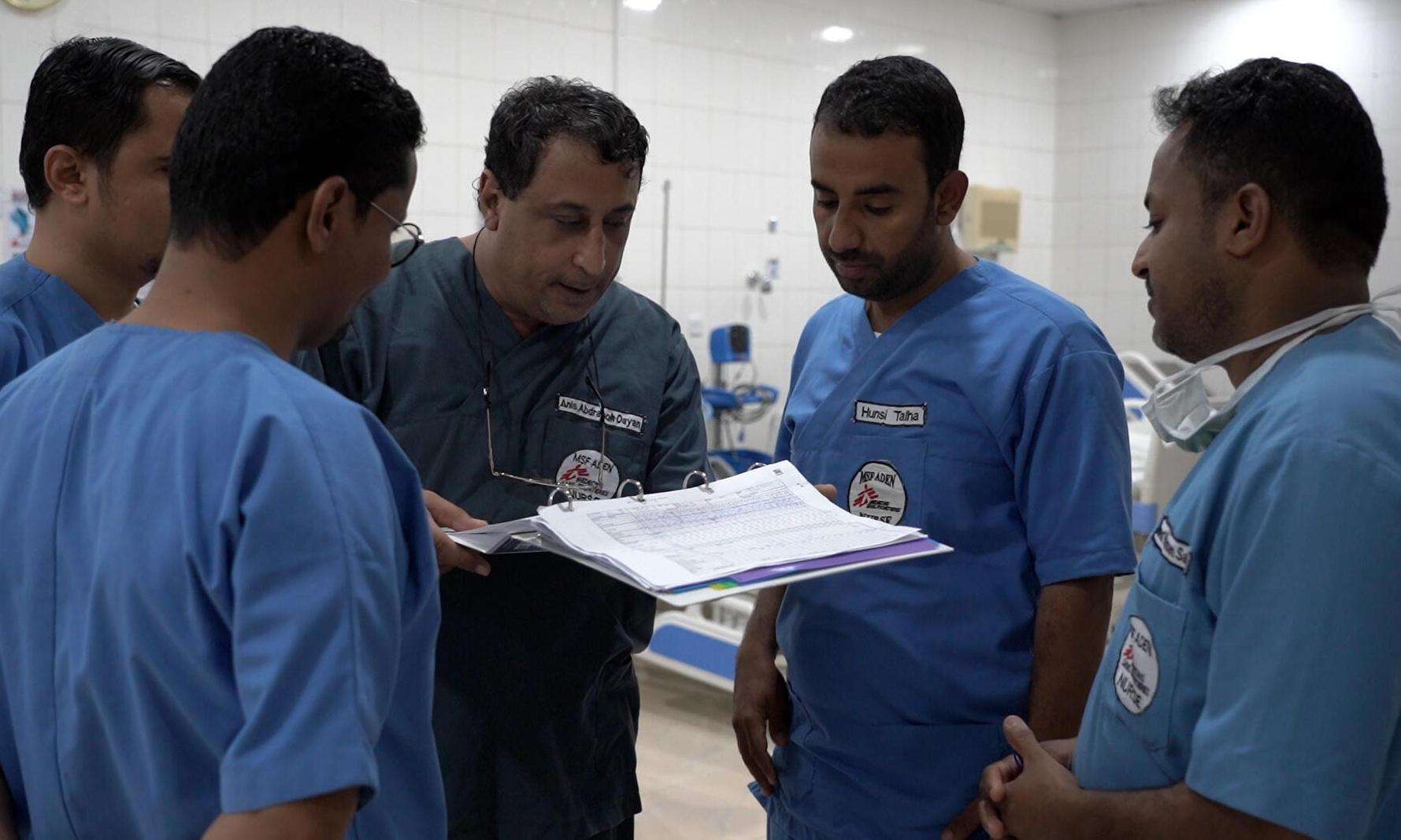
Anis, MSF trauma center, Aden, Yemen
Anis has been working as an intensive care nurse in MSF’s trauma center in Yemen for almost its entire 11-year history. He has reflected deeply on the impact of war and nursing. Anis was inspired to become a nurse after his own medical emergency as a young boy.
The MSF trauma center in the southern coastal city of Aden, Yemen, was opened in 2012 to manage patients suffering acute trauma due to conflict. The hospital provides general and orthopedic surgery (excluding neurosurgery, maxillofacial surgery, and ophthalmology) as well as mental health care, physiotherapy, and laboratory and microbiology services. In 2022, 392 patients received care in the Aden ICU.

When I was a boy, I fell, and started bleeding. I was in so much pain. That's when a nurse in the emergency department received me. He treated me very nicely, eased my fear, bandaged me and gave me medication. I loved nursing from that day on.
I will never forget, as long as I'm alive, a little boy about five years old. He came from a distant village with a gunshot wound to the abdomen. It took a lot of time [for him to reach the hospital] and he lost a lot of blood. The lack of blood led to a lack of oxygen in the brain, resulting in brain dysfunction.
He couldn’t walk and couldn’t talk. As the nursing team in the intensive care department, we developed a treatment plan. In addition to medication, we thought about psychological support, and brought him games and allocated time to sit with him and sometimes with his family, trying to draw him out.
But a miracle happened. It was a beautiful feeling, and most of us cried. He got out of his bed and started walking in front of us.
I started in the inpatient department taking different training and exercises in dressing [wounds], giving injections, and figuring out how to work in accordance with the protocols. Then I moved to the intensive care department, which is a very sensitive department.
The Aden ICU provides the highest level of advanced critical care in MSF. The team sees trauma affecting people’s chest, abdomen, pelvic area, feet, hands, and blood vessels. Many patients have experienced dangerous delays in reaching the hospital, which complicates their condition.
[MSF’s] theoretical and practical exercises and training were at the highest level. I gained more experience in terms of mechanical ventilators for the patient, and how to deal with a patient who suffers from a vascular injury, or after large and complex operations such as laparotomies [abdominal surgery]. I felt like I was experiencing a shift, a turn [in my life]. It was new! It forced me to have more skills.
Challenges remain with any great work you do. The obstacles are many. First and foremost, society's lack of understanding of the concept of nursing—that the nurse's work is limited to giving injections and dressings only. But it's so much more than that. Therefore, the vision must expand and become clearer about the nursing profession, and give it its rightful place, because it is an influential part of this society and all humanity.
The world has so many wars; so many disasters. Grief is ravaging this small world. To plant a smile on a sad face would be a very beautiful thing. You'll feel satisfied; you will feel that you're human in all senses of the word, and that you are practicing your humanity.
Gessica Fleurmond, Tabarre Hospital, Port-au-Prince, Haiti
Gessica Fleurmond’s family knew from early on that she was destined for nursing. Now, Gessica is a highly experienced intensive care nurse, and she and her colleagues help hundreds of trauma patients each year in MSF’s Tabarre hospital in Port-au-Prince, Haiti. She is a strong communicator with a passion for sharing her message.
MSF has worked in Haiti since 1991. The trauma hospital in Tabarre was established in 2019 and provides emergency, surgical, burns, and psychological care, and physiotherapy. The hospital has a 50-bed trauma ICU and an additional 20-bed ICU for severe burns. In 2022 the teams treated 316 people in intensive care.
As a qualified sign language interpreter, she’s able to speak with people who are hearing impaired or have a speech disability. It’s another way she contributes to providing access to care. In Haiti, surging gang-related violence, crime, and road traffic accidents contribute to the consistently high demand for trauma health care.

My ability to become a nurse was discovered by my grandmother and my sister. They thought that I took good care of the ones I loved and that I made sure everything was done as well as possible. I thought that maybe it was my calling. What I enjoy most about my job is when we receive a patient in very bad condition, and we help them get better until they make a full recovery.
Two years ago, a child was admitted here. He was eight years old. He had been the victim of a road accident with very severe injuries to both his legs.
When the patient came in, he was fully aware of what was happening, and he was able to express it. It made quite an impression on me because he was only eight years old. He explained the accident, what he was experiencing, what he felt.
It was really tough. Some of us even cried. And it was especially hard for the parents because they blamed themselves for sending their child to run an errand, so they believed that if they hadn't sent him out, this wouldn't have happened.
The child was in severe pain and needed very high doses of [pain relief medication]. After weeks of care, we were able to save one of his limbs. Now he has fully recovered, and he can easily run and walk with a prosthetic leg.
This made a strong impression on me because he was a child, and it was a very serious accident. He could have died but he was strong, physically, and especially morally. He believed in the future and he didn't give up. It really, really left a mark on me.
In the ICU, we receive patients with head trauma, closed or open abdominal trauma, and also vascular wounds in the upper or lower limbs. They need intensive care because they’re in a life-threatening condition; they need to be closely monitored and they need to be cared for. You do the work, you provide the care, you give the medication, but [if] you already know that this person won't make it, it can be quite difficult and painful—especially when the parents visit.
If the team sees that the patient is not going to make it, we talk to the psychologist, and the psychologist meets with the family. Then, with the doctor and the nurse, we see the family again. We explain what has happened, what we think, what we are going to do. For the family, it's very sad. Sometimes they collapse, crying, but it needs to be done.
We are an intensive care team. We work together in agreement for the good of the patient. There’s a lack of equipment in the hospitals, and there is a lot of frustration among the staff because we feel constrained and limited.
The nurses are competent and qualified, they can work anywhere, sometimes in remote areas replacing a midwife or a doctor. But a lot of equipment is missing. With MSF, I received training on intubation, resuscitation, patient positioning, all of that. With flexibility and adaptability, you learn every day… to work and develop the right skills.
What I wish for this generation of nurses in Haiti is that they be firm, but at the same time gentle; that they have a lot of empathy, love, great ethics, dedication, and also a lot of courage—because it does take courage.
This country is almost pushing us to give up, but if you only look at the negative side, you’ll get discouraged before you even enter the hospital. We need to focus on the patients because they need us. Nursing is a noble profession, and it is a calling. We need to push ourselves and help others, it’s almost like putting ourselves second to take care of others.
Theophilus Tyonongu, Jahun General Hospital, Jigawa state, Nigeria
In Jahun, northern Nigeria, women and girls are admitted daily to the MSF maternity department’s intensive care unit with life-threatening complications in pregnancy or childbirth. Registered critical care nurse Theophilus Tyonongu has followed in his parents’ footsteps to bring his skills and compassion to the unit’s lifesaving work.
An estimated one in four maternal deaths worldwide occurs in Nigeria. Globally, the top five causes of maternal deaths are considered mostly preventable. These include preeclampsia and eclampsia, a form of high blood pressure in pregnancy; postpartum hemorrhage; and severe infection—all of which are commonly seen in MSF’s Jahun ICU. Yet they are only preventable if they are detected early and if people can access skilled care without delay.
MSF teams run the maternity and neonatal departments of Jahun general hospital in collaboration with Nigeria’s Ministry of Health. We provide free and comprehensive obstetric and newborn care and support basic obstetrics in four health centers to reduce complications during pregnancy. In 2022, we admitted 12,621 women to the maternity department, assisted 7,900 births, and treated 1,890 women for severe complications in intensive care.

My parents worked in hospitals and I saw how they helped people. Some of them even became family friends from there. So I saw the impact they made in people's lives and I actually chose to follow this [path].
In Jahun, northern Nigeria, women and girls are admitted daily to the MSF maternity department’s intensive care unit with life-threatening complications in pregnancy or childbirth. Registered critical care nurse Theophilus Tyonongu has followed in his parents’ footsteps to bring his skills and compassion to the unit’s lifesaving work.
An estimated one in four maternal deaths worldwide occurs in Nigeria. Globally, the top five causes of maternal deaths are considered mostly preventable. These include preeclampsia and eclampsia, a form of high blood pressure in pregnancy; postpartum hemorrhage; and severe infection—all of which are commonly seen in MSF’s Jahun ICU. Yet they are only preventable if they are detected early and if people can access skilled care without delay.
MSF teams run the maternity and neonatal departments of Jahun general hospital in collaboration with Nigeria’s Ministry of Health. We provide free and comprehensive obstetric and newborn care and support basic obstetrics in four health centers to reduce complications during pregnancy. In 2022, we admitted 12,621 women to the maternity department, assisted 7,900 births, and treated 1,890 women for severe complications in intensive care.
One of our patients came from a referral facility, which is also a general hospital. A new nurse shift had started and I came earlier than I was supposed to, so I started taking over some basic things, and I took over from the person that brought her in. Unfortunately, went into cardiac arrest just a moment after she was admitted into the ICU. We were able to resuscitate her, and then we managed her from that time until we discharged her. It was a scene of joy.
The best thing about being a nurse is actually seeing the impact of your care in the life of the patient. I’ve been with MSF for roughly two years, and I’ve been working in the ICU for 11 months now. Around Fridays and Saturdays and Sundays, we usually have a lot of very severe cases to manage. The patients we have here sometimes are more critical than those that are being managed in our referral centers. We do not have all the sophisticated equipment we need but there has been a lot of improvement and training. This really helps to strengthen the team, and you see a lot of changes in the team dynamics and in our patient-centered approach.
Nursing in Nigeria is actually developing very fast. There are a lot of improvements; there are a lot of innovations and creativity that is coming from the part of the Nursing and Midwifery Council of Nigeria. But I can see there's a high rate of under-employment, though there’s still a shortage of nurses in the country.
Some nurses' own goals are not met as some may desire. So there's a high rate of emigration, to [places] where they feel they might have a better experience and be able to meet their personal goals better.
What I would like to see in my country is a generation of nurses that are more committed to their work: passionate, and more scientific. I [also want to see] more nurse specialists and academics [so we can] be more outstanding and bring Nigeria to a point where we can be shoulder to shoulder with every other country.
Noami Biswas, Goyalmara Mother and Child Hospital, Bangladesh
As an intensive care nurse in Goyalmara Mother and Child Hospital in Cox’s Bazar, Noami Biswas is committed to providing patient-centered care for severely sick children and their families. In the MSF hospital pediatric ICU, Noami and the multi-disciplinary team treat young children with life-threatening conditions such as severe pneumonia, meningitis, and shock, while also involving their families in their child’s care.
MSF’s Goyalmara Mother and Child Hospital was established in 2017, with a focus on supporting Rohingya refugees and the local Bangladeshi community in Cox’s Bazar with maternity and pediatric care. In 2022, 1,975 children under five years old were admitted for pediatric care, including 1,398 who received intensive care in the pediatric ICU. The hospital also admitted 1,082 newborns for care, including into the newborn ICU.

There was a time when my mom was in the hospital. I saw some nurses there and they were really helpful. They were so caring. They inspired me.
I thought, I can [be] like them. There was a time in Bangladesh that nursing was not a preferable profession. But nursing in Bangladesh is developing now. After COVID we were highlighted, and now people like us.
The best thing about being a nurse is connecting with patients and their families and helping them in their bad times when they need us the most. We involve them in everything from the beginning. With patient feeding, we involve the mother all the time because they need to know how to feed the baby. We explain to the patient, mother, and family—fathers also.
Last year there was a patient with meningitis. She was admitted to our hospital, and she was dying. And we were [initially] going to discharge her with palliative care. But we tried [to treat her].
Her father was there. We involved him in our treatment. He was constantly sitting with us, helping with the baby’s positioning and everything. After 23 days, she healed, and she went home. It’s a very successful story for me.
The hardest thing about being a nurse is when you are seeing people dying. This is really painful for us.
In the ICU there are so many critical patients. We have ten beds and two isolation beds, and we are almost full every time. We are giving cardiopulmonary resuscitation (CPR) and manual ventilation using a bag-valve-mask. So, this is different from the normal ward.
I want people to know that nursing is a great profession and we nurses really work hard, so that someone’s loved one can heal and go home safely.
Nursing is a great job. We need more nurses with compassion and a very strong mentality to serve not only the job, but the people [too]. I think we need nurses like this who are willing to do something for our country, for our community and our people. To the younger nurses I say, come.
How you can help
Not everyone can treat patients in the field. But everyone can do something.
Some humanitarian crises make the headlines—others don’t. Unrestricted support from our donors allows us to mobilize quickly and efficiently to provide lifesaving medical care to the people who need it most, whether those needs are in the spotlight or not. And your donation is 100 percent tax-deductible.