The deadliest Ebola outbreak on record killed more than 11,300 people and infected nearly 30,000 in West Africa from 2014 to 2016. Though Ebola was not new—it was first identified in 1976—such a massive outbreak of the viral disease was unprecedented.
Doctors Without Borders/Médecins Sans Frontières (MSF) immediately launched an emergency response when the outbreak was confirmed in Guinea, and later expanded operations to Sierra Leone and Liberia as the virus spread, but no antiviral treatments or vaccines existed at the time. We had few tools with which to fight such an enormous outbreak.
The lessons learned during the response have helped to inform the development of new strategies and treatments to tackle new outbreaks of Ebola—and in many ways changed MSF's approach to treating the virus. On the 10-year anniversary of the outbreak, renowned Ebola expert Dr. Michel Van Herp looks back at the biggest Ebola outbreak ever and answers five key questions.
Why was this outbreak different?
Never had Ebola outbreaks happened in so many countries at the same time. The virus spread in Guinea, Sierra Leone, and Liberia, but there were also cases in Senegal, Mali, and Nigeria. It was also the first time that Western countries, like Italy, Spain, the United Kingdom, and the United States, had cases of Ebola.
The scale of this epidemic was absolutely unheard of. When it was finally over in March 2016, more than 28,000 people had been reported to be infected, of which 11,000 died. Before this epidemic, the largest Ebola outbreak had 425 infected people! Everybody, including MSF, was completely overwhelmed by this outbreak.
Timeline: 2013
December 2013
A mysterious disease appeared in Guinea.
March 21, 2013
Laboratory tests confirmed it to be Ebola. It spread in the areas bordering Guinea, Liberia, and Sierra Leone, and quickly affected all three countries. MSF deployed teams to Guinea and Liberia.
April 2013
Eighty-three people had died, and MSF described the outbreak as unprecedented. The worst was yet to come, however, with the epidemic spreading faster than the response by the international community. MSF responded in all three countries but was not able to meet all of the needs.
June 2013
MSF publicly stated that the epidemic was out of control and called for urgent action by the international community.
Was the response to this outbreak also different?
For almost six months, the world tried to ignore this outbreak. Only by the end of the summer of 2014 did other governments and aid organizations finally start to help.
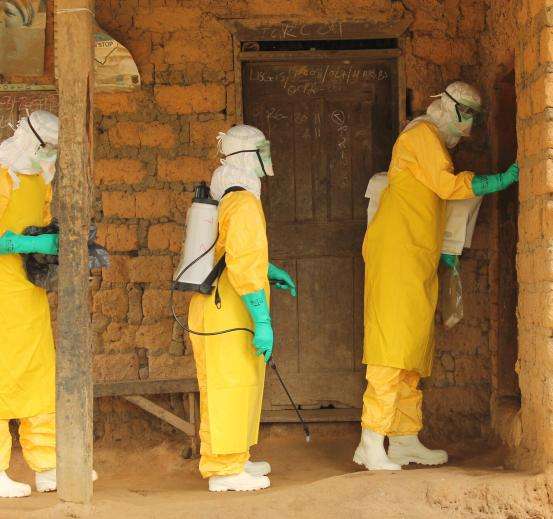
At the time, there were no treatments for Ebola; patients would be admitted to an Ebola clinic, mainly to avoid infecting other people. In earlier outbreaks, a family member could accompany the patient. However, in 2014, to admit the huge number of patients, very big structures had to be built. The safety procedures had to be extremely strict, and it was impossible to allow family members. This large-scale approach scared patients and their families.
By the end of 2014, dozens of aid organizations, most of them inexperienced with Ebola, were involved in different aspects of the response. Coordinating all those organizations in multiple places in multiple countries was extremely challenging. Some governments turned to authoritarian tactics to force patients and their families into compliance, which scared them even more.
The focus on the patients and their families that had been so key to contain previous outbreaks was completely lost in the enormous machine that the Ebola response had become.

How did the Ebola response begin 10 years ago?
When we read the reports of people dying of an unknown disease in Guinea early in 2014, we thought this was probably an outbreak of Ebola, even if that disease was extremely rare in West Africa. We sent our Ebola teams. At that time, MSF was one of the very few organizations with experience in Ebola outbreaks. But it became clear that this outbreak had been slumbering for months and was already present in more places than anybody was used to dealing with.
The outbreak happened in a place in the world where no one expected Ebola, in an area that didn’t interest the authorities, and no one was ready to deal with it. It took governments, United Nations agencies, and aid organizations a very, very long time to take the outbreak seriously. MSF frantically rang the alarm bell multiple times, but nobody seemed to listen.
2014
April-May 2014
An apparent lull in new cases inspired cautious hope, but MSF teams continued to see new Ebola patients.
Challenges arose when a fearful public struggled to reconcile traditional and religious beliefs with the strict medical protocols required to halt the spread of the disease. Mounting public anxiety culminated in violent protests in one area of Guinea and an Ebola treatment center was temporarily closed.
June-July 2014
Ebola patients had been identified in more than 60 locations in Guinea, Sierra Leone, and Liberia. Despite the human resources and equipment deployed by MSF in the three affected countries, we were no longer able to send teams to new outbreak sites. In a press release, MSF said, “The WHO, the affected countries, and neighboring countries must deploy the resources necessary for an epidemic of this scale.”
Did we learn anything from it?
Many of the things that we consider 'lessons learned' are things we knew before 2014 but that were forgotten. But we have also learned new things. We learned how we could take a simple, oral swab of deceased people, to test whether they had died of Ebola. This allowed us to understand the dynamics of the epidemic better.
We also learned from organizing the clinical studies, so we were faster during the 2018 outbreak in the DRC. In DRC, we found treatments with antibodies for the Zaire strain of Ebola.
2015-2016
January 2015
The epidemic began to slow down, but it was not over yet. Starting in late December 2014, research was carried out for developing treatment, diagnostics, and a vaccine. In this first year of the response, close to 500 health professionals, including 14 MSF workers, had lost their lives in the fight against the Ebola virus.
November 7, 2015
The end of the outbreak was declared in Guinea. The last identified patient, a newborn, left the Ebola treatment center at the end of November.
January 14, 2016
The end of the epidemic was declared in Liberia. This was also the official end of the epidemic as a whole. After battling Ebola for two years, MSF switched focus to a new group of people who need special care, the Ebola survivors.

What needs to be done to prepare for future outbreaks?
There are very concrete things we can improve. We should again allow a family member to accompany a patient in the Ebola clinic, since we can protect them better now with vaccination and drugs for pre-exposure prophylaxis.
Very sick patients should receive an antibody treatment much faster. Antibodies can be real lifesavers, and the sooner a patient receives them, the better they will work. We must adapt our models to make the best use of this option. And we need to continue looking for other treatments. The Ebola virus can provoke an inflammatory response that is so strong that it can kill the patient. If we had a drug to calm down that inflammatory response, we could save more Ebola patients.
We also must improve the follow-up of patients after their recovery. The virus can linger in the brain, the eyes, and the testes of survivors. Another type of drug, antivirals, can clean up the virus from these places. And six months after their full recovery, Ebola survivors should get a shot of the vaccine to give their immune system another boost.
In the last 10 years, we have certainly made errors when we responded to Ebola outbreaks. Some errors were forced, some were unforced. But in general, we clearly have made progress, and there are good options for even more progress. The odds for a patient with Ebola in the next outbreak will be much better than they were 10 years ago.