More than 22 million people were estimated to need humanitarian assistance in Ethiopia in 2022, according to the UN. Many faced the tragic consequences of conflict, particularly communities in the regions of Afar, Amhara, Tigray, and Southern Nations (SNNPR).
At the same time, natural disasters pushed people’s coping mechanisms to their limits. Communities across the vast Somali region experienced what is reportedly the worst drought in forty years, and when floods struck the Gambella region more than 180,000 people were displaced from their homes and health facilities suffered extensive damage.
Doctors Without Borders/Médecins Sans Frontières (MSF) responded to the emergency medical and humanitarian needs of people in all these regions, including those impacted by deadly neglected tropical diseases endemic to. Here, MSF staff describe what they have witnessed and the impact of humanitarian action in Ethiopia.

Sitti Zone, Somali region: Mobile stabilization clinics
“For three months, between July and September, we responded to a terrible emergency in Sitti Zone in the Somali region of Ethiopia, an area cyclically afflicted by a combination of drought and floods, loss of livelihoods, as well as nearby conflict and displacement,” said Anna, MSF’s project coordinator.
“The challenge was to find a way to respond to the enormous needs of communities spread across a huge area. MSF ran mobile nutrition stabilization clinics in several locations that carried out screenings and a first response to malnutrition with therapeutic food. The project was aimed at children, but severely malnourished adults were also provided with medical care and patients with complications were transported back to the inpatient therapeutic feeding facility MSF supported in Asbuli for more advanced care.

“During the intervention, almost 2,600 people received medical consultations. We know that our intervention was limited, as we could only respond to the needs of people we could reach or who could reach us. However, I consider the intervention successful because it was launched at the right time and, together with the work of regional authorities and other organizations, undoubtedly saved lives and helped bridge the hunger gap for people until the rains finally came along,” said Anna.
Liban zone, Somali region: Cholera response
The peak of the malnutrition season passed by November. As MSF’s emergency malnutrition response started to phase out, other MSF teams were preparing to expand activities in response to a cholera outbreak. Medical teams started providing hands-on training on cholera case management to local medical staff. MSF logistics and water and sanitation experts were also ensuring access to safe water and hygiene—their critical expertise often happens in the shadows of the organization’s medical action but is indispensable.

Conflict and drought spark a deadly malnutrition crisis in Ethiopia's Afar region
View the timelineTeams travelled for five days to reach Kersa Dula in Liban zone to respond to the rapidly spreading outbreak. Cholera is a disease that can precipitate or aggravate malnutrition.
“Once in place, the team rushed to set up a cholera treatment unit with latrines and showers. As numbers of people affected increased in Liban zone, the team also built a stabilization unit in Baliat.
“Separately, around 75,000 people live in Adeley camp for people who are displaced, the camp most affected by the cholera epidemic, and the team set up cholera treatment centres, hand washing points, built 12 latrines, and a water treatment plant to allow people access to clean, safe drinking water. Oral rehydration points were also set up within the camp,” said Najah Aden Mire, MSF’s water and sanitation manager.
With ongoing reports of cholera and measles, the potential for further outbreaks including other diseases, is high. The team worked in partnership with the Regional Health Bureau providing training on case management and infection prevention and control to local health staff.

How MSF is tackling cholera outbreaks in 11 countries
View the timelineAmhara region: Communities affected by conflict
In the rural areas of northern Amhara affected by conflict, people have experienced violence, loss of property and assets, and struggle to access basic services such as health care due to disrupted systems. Months of conflict in the region have exhausted people’s coping mechanisms.
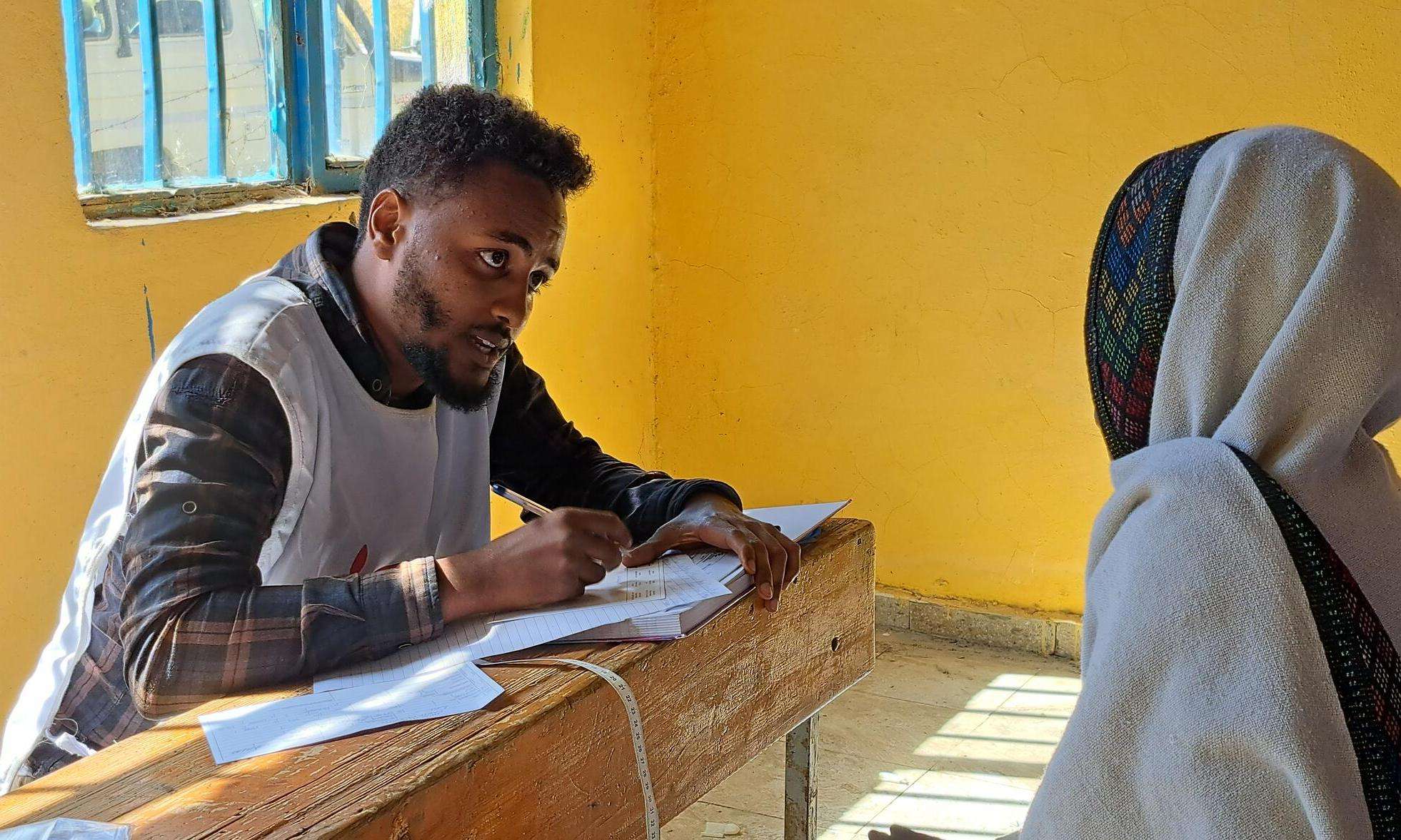
“We see very high needs here. Most of our patients are affected by depression, some have lost relatives or their houses have been destroyed, others might have lost their livelihood,” said Demeke, supervisor for psychosocial services.
“A number of patients we see are survivors of violence or may have witnessed traumatic events and are now suffering from post-traumatic stress disorder.
“Frehewot was one such patient. The six-year-old girl was brought to our clinic by her parents after she had started bedwetting. It became apparent that her symptoms had developed suddenly after she had witnessed violence and seen dead bodies lying on the side of the road,” he said.
Among the essential health care services which MSF mobile health teams offer, women’s health and psychosocial support are central to the response.
“Our medical teams have been treating survivors of sexual and gender-based violence. Survivors are offered medical care as well as psychosocial support,” said Noortje, one of MSF’s mobile clinic doctors.

“The stories we hear are quite similar. I will share the example of a 45-year-old woman who was sexually assaulted one month ago. I’ll call her Lilian,” said Noortje.
“There is a lot of stigma attached to sexual violence; for every person that seeks treatment, many others will not. When Lilian first came to the clinic, she was experiencing unexplained pains in her abdomen. People worry about serious infections such as HIV so taking time to explain the risks and post exposure prophylaxis makes a huge difference.
“After receiving medical care, I could tell she was already feeling relieved and reassured,” said Noortie.
Kule camp: MSF has no borders
In Kule camp, where more than 50,000 people from South Sudan now reside after having sought refuge, MSF medical teams offer primary and secondary health care services and treat both outpatients and inpatients.
“I drove 45 minutes to get my daughter and wife to a doctor,” said Temesegen, a state employee of the Refugees Returnees Service. “This is not the first time I have come to MSF’s hospital. In 2019, I was admitted in critical condition. At the time I had first visited another health center, much closer to where I lived, to seek treatment but when I was not improving I was told to try another organization called MSF, in Kule camp. Even though there are other options, MSF provides the best quality service,” he said.
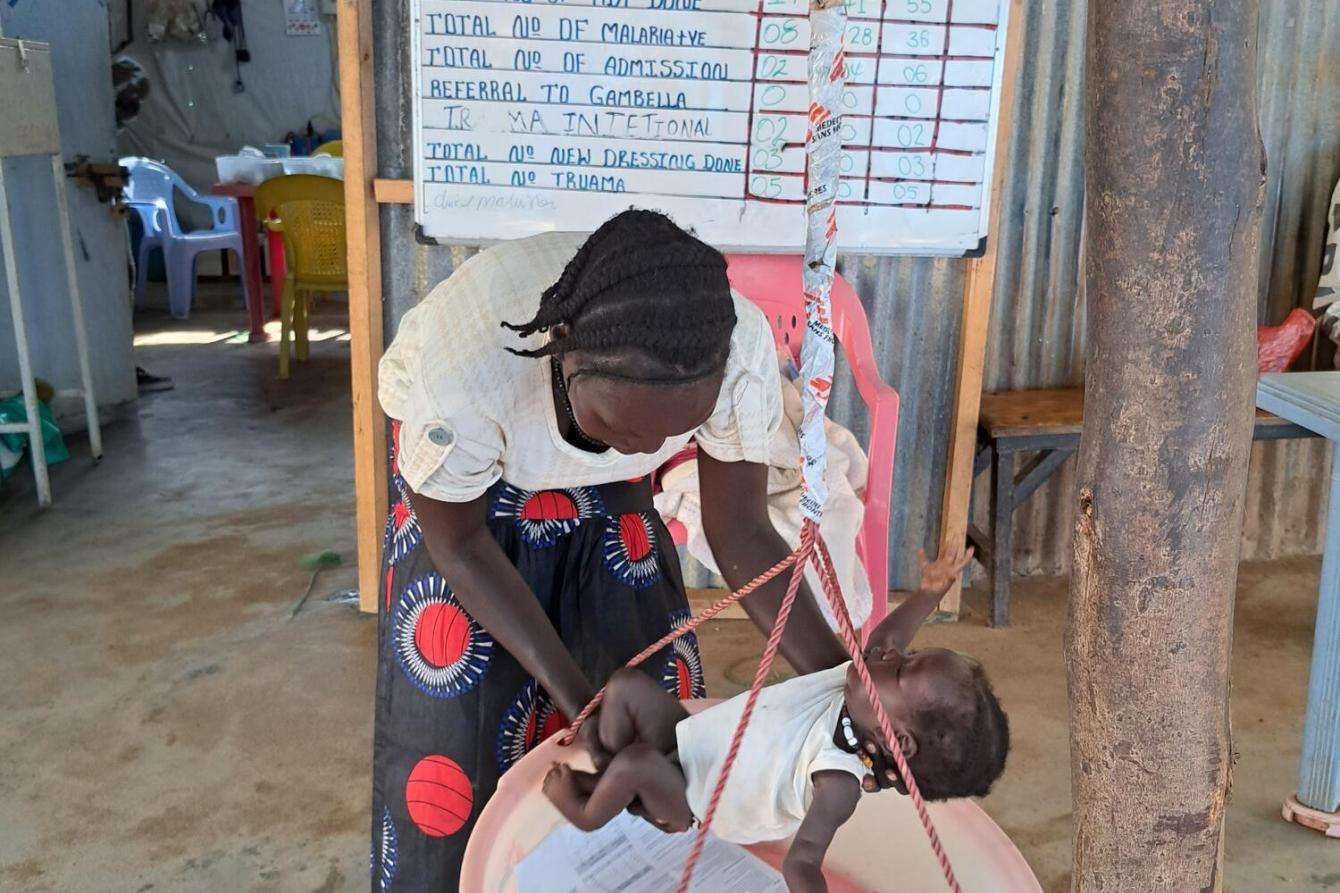
“Our patients are not only South Sudanese refugees,” said Hailemariam, a doctor working in Kule health center emergency room. “We also provide services for the host community. Many work here for different aid organizations, as well as for Ethiopia’s organization for refugees. People also come from other refugee camps; it can take them up to four hours to get here. Most of the patients are children under five and pregnant women. We have a registration form on which we record where people come from – but specifically for medical purposes because at MSF we make no distinction in treating patients. I am also a stranger, I come from Addis, other colleagues are from Gambella, at MSF there are no borders.”
Abdurafi, Amhara region: Snakebite
Both snakebite envenoming and kala azar, the second deadliest parasitic disease in the world, are endemic in Ethiopia and are among the world’s most neglected diseases.
“We had just reopened our clinic in Abdurafi, when, three days later, a 12-year-old boy was brought to us in close-to-death condition from the hospital in Metema. He had suffered snakebite envenoming on his right foot in Abdu, the village where he lived 100 kilometres [about 60 miles] from Metema,” said Kassaye, MSF’s medical activity manager in Abdurafi.
“The doctors there were able to put him in an ambulance and send him to Abdurafi, the facility where, since 2015, MSF offers quality, free anti-venom treatment. He arrived in very poor condition. Even his brothers did not believe he would recover. He was vomiting blood, his pulse was barely discernible, he was in haemorrhagic shock and semiconscious.
“We didn’t waste time. We placed him on two drips, one with the anti-venom, the other with rehydration fluids. One hour later, he was still vomiting so we gave him a blood transfusion and more anti-venom. Two hours later, his blood pressure had recovered, but he was still bleeding so we gave him another dose of anti-venom. We tried everything. We used 12 vials of anti-venom to treat the child. It was truly amazing that the boy recovered.”

“I joined MSF because of its impact on the lives of people like this boy, and its principles. The one I find the most vital is impartiality. It is at MSF’s core—we treat everybody regardless of who they are or where they’re from.
“I remember back in November 2019, on the border with Sudan, not far from the Abdurafi clinic- one day, a Sudanese man came to our health center. He was ill with kala-azar, a deadly disease transmitted by the sand fly that MSF teams treat in this clinic.
“However, we could not understand each other because he could not speak a word of Amharic but only Arabic. We went looking for a translator in town and sure enough found someone who could translate. The man was treated and eventually recovered and was discharged. That is what MSF stands for. We don’t discriminate, we don’t look at where people come from, what their religion is, what allegiance they have,” said Kassaye.
MSF has been working in Ethiopia for 37 years, providing medical assistance to millions of people affected by conflict, epidemics, disasters, or with limited access to health care in collaboration with Ethiopian authorities at local, regional, and national levels. All our activities are guided by humanitarian principles of independence, neutrality, and impartiality.
How you can help
Not everyone can treat patients in the field. But everyone can do something.
Some humanitarian crises make the headlines—others don’t. Unrestricted support from our donors allows us to mobilize quickly and efficiently to provide lifesaving medical care to the people who need it most, whether those needs are in the spotlight or not. And your donation is 100 percent tax-deductible.