In Central African Republic (CAR), decades of instability and conflict have contributed to a dearth of essential medical care for many pregnant women and newborn babies. Doctors Without Borders/Médecins Sans Frontières (MSF) is responding with free emergency obstetric care for women and newborns across the country. We are also training ministry of health staff and renovating and equipping medical facilities so they can provide a good standard of care. In 2021, MSF teams assisted nearly 19,600 births, including 1,020 Cesarean sections, while 1,900 newborn babies were treated in MSF-supported neonatal units across the country.
"Many women do not go to a health center for their delivery but give birth at home,” said Adèle Guerde-Seweïen, an MSF midwife at Bangui's community hospital, known as the CHUC. “In this situation, complications can easily lead to the death of mother or child."

An extreme situation
A scream, louder than all the other raised voices, rings out across the hospital ward. A woman has just learned of the death of her pregnant sister. Minutes earlier, she had been rushed to hospital and taken straight to the operating theater. The medical team did their utmost to stabilize her but only managed to save her baby.
"This tragedy would not have happened if she had had access to medical care in time," said Guerde-Seweïen.
Maternal and neonatal health is a major health emergency in CAR. The country’s maternal and child mortality rates are among the highest in the world. According to the most recent statistics from the World Bank, women are 138 times more likely to die of pregnancy and delivery complications in CAR than in the European Union, while a baby in CAR is 25 times more likely to die before its first birthday than if it had been born in Europe.

Families of patients admitted to the maternity ward stay on the premises of the Community Hospital Center in Bangui. Central African Republic, 2022 © Barbara Debout
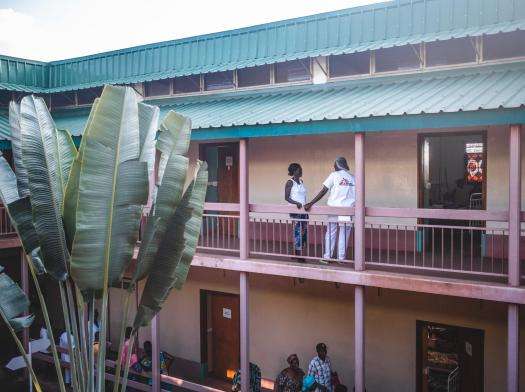
MSF nurse Virginie Abdouramane (right), is talking to a patient at the MSF-supported maternity of the Community Hospital Center in Bangui. Central African Republic, 2022 © Barbara Debout
15 gynecologists for six million inhabitants
"In CAR, to be born or to give birth is to take a risk," said Professor Norbert Richard Ngbale, an obstetrician-gynecologist in the CHUC’s maternity and neonatology department. "There are only about 15 gynecologists in the country, for a population of six million. There is a massive lack of qualified staff, especially in rural areas, where you mostly have traditional birth attendants who are not trained to detect complications.”
Most maternal deaths in CAR are related to unsafe abortions, pregnancies in girls and women who are too young to give birth, and unsafe home births. Many of these tragedies could be avoided if health care like pregnancy support and family planning was available. CAR’s chronic medical emergency is also fueled by extreme poverty: while maternal and child health care is officially free in CAR, in practice it is often only available to those who can afford to pay.
“In a country where 70 percent of the population lives on less than $2 a day, every decision must be weighed up financially, even if it means putting one's health at risk," said René Colgo, MSF head of mission in CAR. "For patients, going to the hospital is an expense. They don't have money to pay for prenatal care, nor for transport to hospital, let alone for the delivery. Many women think it is better to go to hospital at the last minute, if at all. Supporting the provision of free care is therefore vital."

Central African Republic: Women share stories of survival
Read more"This time, I wanted to avoid any risk”
As a mother of eight who experienced complications in childbirth with her seventh baby, Carine Dembali did not want to risk arriving too late at the hospital this time.
"With the exception of my first child, I have always given birth at home due to lack of money," she said. "Last time, there was a problem. My baby came out but the placenta didn’t. My family rushed me to Castor’s [a hospital with a maternity ward previously managed by MSF], where I didn't have to pay anything. That’s why this time I wanted to avoid any risk. I went to the hospital near my home before the delivery. They saw that the cord was threatening my child and I was brought here for a Caesarean.”

The CHUC’s maternity and neonatal wards, which were fully renovated by MSF before opening in July 2022, provide emergency care to pregnant women and newborns in critical situations. From mid-July to Mid-December, teams of MSF and of the Ministry of health provided care to 3,084 pregnant women, and 860 babies were admitted in the neonatal ward, including 239 born preterm.
Few hospitals in the country provide a similar service, which includes an intensive care unit for premature babies and newborns who have trouble breathing and other complications.
Archange, who was born at just 28 weeks (compared to a normal gestation period of 38–40 weeks), fought for his life for 45 days in the intensive care unit of the CHUC. The medical team was so impressed by his fight to survive that they nicknamed him “little general.”

"He weighed 800 grams [1.7 lbs] at birth,” said his mother, Stephanie. “His twin sister unfortunately died after two weeks, and I thought I was going to lose him too.”
The MSF team persuaded her to try “kangaroo care,” where premature babies are held close to their mother’s bodies 24 hours a day. The prolonged skin-to-skin contact keeps them warm, maintains their emotional balance and ultimately improves their chances of survival.

Forgotten Emergencies 2022: MSF responds
Read more“When he came out of intensive care, we started the ‘kangaroo method,’” said Stephanie. “I was stressed and not convinced. But soon I saw that he was getting better and better, and that his health was improving. Today he weighs 1.5 kg [3.3 lbs]. Soon I'll be able to go home with him.”
More support is needed
While MSF teams continue to provide urgent lifesaving care in CAR, more support is needed to bring these essential services to women and babies countrywide. "The situation calls for ambitious investment by all international partners to strengthen access to reproductive health services,” said Colgo. “It is unacceptable that so many women’s and babies’ lives are being lost every day for reasons that are so easily preventable."




